The Abstracts in their Short and Long Versions are below the Figures.
SHORT VERSION – < 350 words
*Authors: Curtean A1, Lisciandro GR2
1 Cat Care Clinic, Ormond Beach, Florida USA
2 Hill Country Veterinary Specialists, Spicewood, Texas USA
*We acknowledge Dr. Geoff Fosgate, DVM, PhD, DACVPM for helping with the study’s design and statistical evaluation.
Title: Comparison of Point-of-care Ultrasound Small Intestinal Jejunal Measurements in Clinically normal and GI disease-affected Cats During AFAST
Introduction: Point-of-care ultrasound (POCUS) is becoming common practice as part of initial patient assessment. The standardization of AFAST used not only for the detection of free fluid and its fluid scoring system, but also its target-organ approach for soft tissue abnormalities has led to “add-on” POCUS skills. Feline gastrointestinal (GI) disease is common and having first line veterinarians screen using POCUS might identify such cats. The objective of this study was to compare AFAST jejunal measurements and the muscularis:submucosa ratio between clinically normal and GI disease-affected cats to investigate their ability to differentiate these animals.
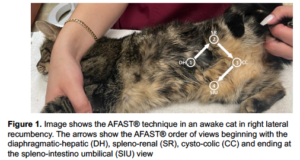
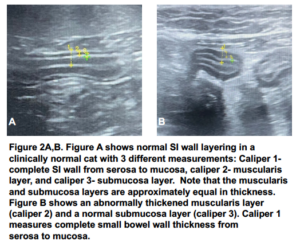
Methods: Client-owned cats >12-months old that presented for vomiting, weight loss, anorexia, or any combination of these GI signs were included in the study. Clinically normal cats were client-owned cats >12 months old presenting for wellness exams. Following physical exam, cats were evaluated with AFAST followed by jejunal muscularis and submucosal measurements. Jejunal measurements and the muscularis:submucosa ratio were compared between GI disease-affected and clinically-normal cats.
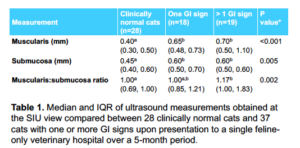
Results: Twenty-eight clinically normal and 37 GI disease-affected cats were enrolled over a 5-month period. Median (standard deviation) and statistical significance for clinically normal and GI disease affected cats, respectively, were weight (kg) 5.4 (1.3) and 4.7 (1.3) P=0.030; temperature (C) 38.4 (0.6) and 38.5 (0.7) P=0.598. Median (interquartile ranges) and statistical significance, respectively, were age 4 (2,7) and 13 (9, 15) P<0.001; BCS (1-9) 5.5 (5, 6) and 5 (4, 6) P=0.007; pulse (/min) 185 (174, 186) and 180 (175, 186) P=0.509; respirations (/min) 30 (27, 39) and 36 (30, 41) P=0.092. POCUS measurements for clinically-normal cats were muscularis (mm) 0.40 (0.30, 0.50), submucosa (mm) 0.45 (0.40, 0.60), and the muscularis:submucosa ratio 1.00 (0.69, 1.00). The GI disease-affected cats had larger muscularis and submucosa measurements compared to clinically normal cats (P<0.05), but the muscularis:submucosa ratio was only significantly larger in cats with >1 GI sign at presentation. None of the study cats had AFAST-detectable free fluid.
Conclusion: There were differences between the clinically-normal and GI-affected cats in their jejunal wall measurements as expected, but for cats with only a single GI sign, there was no difference in the muscularis:submucosa ratio.
LONG VERSION – < 450 words
*Authors: Curtean A1, Lisciandro GR2
1 Cat Care Clinic, Ormond Beach, Florida USA
2 Hill Country Veterinary Specialists, Spicewood, Texas USA
*We acknowledge Dr. Geoff Fosgate, DVM, PhD, DACVPM for helping with the study’s design and statistical evaluation.
Title: Comparison of Point-of-care Ultrasound Small Intestinal Jejunal Measurements in Clinically normal and GI disease-affected Cats During AFAST
Introduction: Point-of-care ultrasound (POCUS) is becoming commonplace in general and emergency and critical care practice as part of initial patient assessment. The standardization of AFAST used not only for the detection of free fluid and its applied fluid scoring system, but also its target-organ approach for soft tissue abnormalities have led to “add-on” skills such as characterizing the caudal vena cava, the detection of free air, the evaluation of gastrointestinal motility, and measurements of the urinary bladder for its volume estimation and thus over time, non-invasive urine output. Gastrointestinal (GI) disease is common in cats and having first line veterinarians screen for small intestinal disease using POCUS might identify such cats. The objective of this study was to compare AFAST jejunal measurements and the muscularis:submucosa ratio between clinically normal and GI disease-affected cats to investigate their clinical utility in differentiating these animals.
Methods: Client-owned cats >12-months old that presented for vomiting, weight loss, anorexia, or any combination of these GI signs were included in the study. Clinically normal cats were client-owned cats >12 months old presenting for wellness exams. Following their physical exam and before any further interventions, cats were evaluated with AFAST followed by jejunal muscularis and submucosal layer measurements at the AFAST spleno-intestino umbilical view. Jejunal measurements and the muscularis:submucosa ratio were compared between GI disease-affected and clinically-normal cats.
Results: Twenty-eight clinically normal and 37 GI disease-affected cats were enrolled (43% versus 51% female and 79% and 65% domestic short hair, respectively). Median (standard deviation) and statistical significance for clinically normal and affected cats, respectively, were weight (kg) 5.4 (1.3) and 4.7 (1.3) P=0.030; temperature (C) 38.4 (0.6) and 38.5 (0.7) P=0.598. Median (interquartile ranges) and statistical significance, respectively, were age 4 (2,7) and 13 (9, 15) P<0.001; BCS (1-9) 5.5 (5, 6) and 5 (4, 6) P=0.007; pulse (/min) 185 (174, 186) and 180 (175, 186) P=0.509; respirations (/min) 30 (27, 39) and 36 (30, 41) P=0.092. Median (interquartile range) POCUS measurements for clinically normal cats were muscularis (mm) 0.40 (0.30, 0.50), submucosa 0.45 (0.40, 0.60), and the muscularis:submucosa ratio 1.00 (0.69, 1.00). The GI disease-affected cats had larger muscularis and submucosa measurements compared to clinically-normal cats (P<0.05), but the muscularis:submucosa ratio was only significantly larger in cats with >1 GI sign at presentation. None of the study cats had AFAST-detectable free fluid. The number of AFAST views for the clinically normal and GI disease-affected cats, respectively, included the diaphragmatico-hepatic, 23/28 and 34/37; spleno-renal, 27/28 and 34/37; cysto-colic, 26/28 and 36/38; and spleno-intestino umbilical, 28/28 and 37/37.
Conclusion: There were differences between the clinically-normal and GI disease-affected cats in their jejunal wall measurements as expected, but for cats with only a single GI sign, there was no difference in the muscularis:submucoas ratio.