As you may know, my wife Stephanie Lisciandro, DVM, DACVIM (SAIM), was trained at The Animal Medical Center in the mid 1990s. There she was taught to look at the caudal vena cava (CVC) and hepatic veins for right-sided volume overload and right-sided congestive heart failure by Dr. Richard “Scotty” Scott. In 2005, we created AFAST® and TFAST® while Stephanie was working as an internist at a referral practice, and then doing mobile ultrasound and consulting in San Antonio, Texas. She had little interest in AFAST® and TFAST® until 2010 when she had enough local referring practices begin asking about what her husband, Greg (me), was doing with AFAST® and TFAST® ultrasound at the Emergency Pet Center in San Antonio.
So, she asked me…When I explained to her what we were doing, how we were performing the AFAST® and TFAST® examinations, the AFAST® and TFAST® information we were acquiring, and how we recorded our AFAST® and TFAST® findings on Goal-directed Templates, she suggested we add imaging and characterizing the CVC and hepatic veins. This was far in advance (years) of any other veterinary point-of-care ultrasonographers considering such a notion. In fact, we trained the groups out of Canada and Europe on how to image and characterize the CVC. So, I give all the CVC credit to my wife Stephanie, on making this paradigm change in veterinary medicine. We hope you enjoy this ECC and IM Blog.
Some Clinical Pearls for Imaging the Caudal Vena Cava.
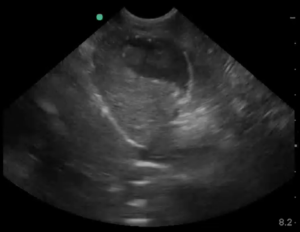
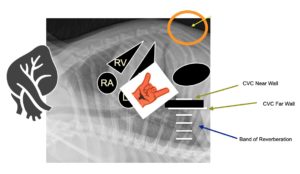
The above figure shows the classic AFAST® and TFAST® DH view and the location of the CVC, along with the narrow column of reverberation-mirror artifact extending from the longer CVC far wall through the far field.
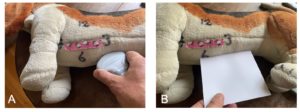
Holding the probe.
The key is holding the probe so your scanning plane cuts through the caudal vena cava (CVC) along its longitudinal scanning plane. Holding the probe with your “hand on top” rather than like a pencil keeps the scanning plane “true.”
Best for success – you must be longitudinal as shown here!
Note that the hand is on “top of the probe” with the thumb on the marker and the index finger on the other end as shown in A). By doing so, the scanning plane is like the piece of paper in B) and in a longitudinal plane. By holding the probe in this manner, you can fan in a “true” longitudinal plane. Staying “true” to the longitudinal plane will give you a good CVC image.
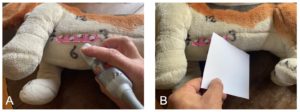
This is a fail – holding like a pencil obliques the CVC and won’t be accurate!
Note that the probe is held like a pencil as shown in A). By doing so, the scanning plane is like the piece of paper in B) and obliqued which will not provide a good image of the CVC and one accurate for measuring.
A final comparative image!
Note the difference in how the probe is held in the “Good!” and “Bad!” images.
Rocking cranially to get the caudal vena cava.
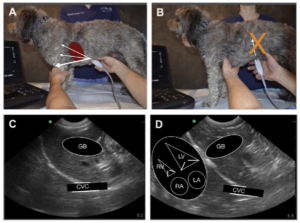
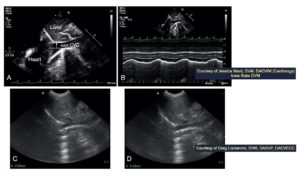
The image of from the 2nd edition of our textbook, a great resource for you, that may be purchased through Amazon. Note in A) the probe marker is directed far cranially bringing the white curved line along the diaphragm close to the probe head, close to the near field, as shown in C) and D). In contrast in B), the probe is directed toward the spine, which will generally be a fail for imaging the CVC, because it will bring the stomach and its shadowing through the CVC area of interest. In D) the overlay shows you the orientation of the heart chambers relative to the diaphragm. Note the left heart is along the diaphragm and this holds true for all quadrupeds. In contrast, people (bipeds) have the right heart closest to the diaphragm.
Additional Pearls for Imaging the CVC are 1) The CVC is “a Texas Longhorn away” from the “cardiac bump”, where the heart is opposed to the diaphragm, and 2) increasing depth to find and then follow the short column of reverberation artifacts to the diaphragm to locate the CVC. Note the column of bars are more narrow than the far wall of the CVC.
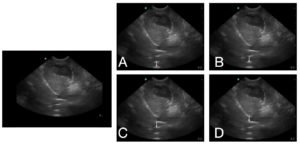
Quiz – Can You Properly Identify the CVC?
Note the image to the left without any arrows; and then the arrows showing the possible location of the CVC in A) through D). Which image correctly has the arrow where the maximum CVC height is located (A-D)? The answer at the bottom of this Blog.
Measuring the CVC Height
Measuring the maximum height (it’s not a diameter, there is no circle) and using our CVC chart to categorize as fluid responsive (bounce), fluid starved (flat), or fluid intolerant (FAT). The best manner to find the CVC maximum height is to image the CVC over several seconds because it has respirophasic variation, then freeze and roll the track ball through frames finding its maximum height. Although, keep in mind that the “eyeball characterization” of the CVC trumps the maximum height.
The *FASTVet CVC Maximum Height Rule is easy to remember: for cats the maximum CVC should be < 0.5 cm; for small dogs < 9 kg the CVC maximum height should be < 1 cm; and for larger dogs > 9 kg the CVC maximum height should be < 1.5 cm
*So Remember Greg’s Rule for Maximum CVC Heights as < 0.5 (cats) to < 1.0 small dogs to < 1.5 large dogs
B-mode or M-mode for measuring the CVC maximum height? You may use B-mode or M-mode; however, B-mode is usually much easier (unless you are a cardiologist or use M-mode a lot).
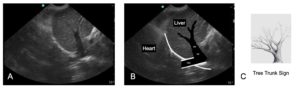
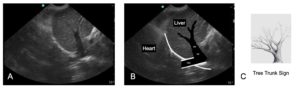
Hepatic Venous Distension and the “Tree Trunk Sign”
We have shown and published (Chou et al. 2021) the “Tree Trunk Sign” as 96% specific and 84% sensitive for the presence of right-sided congestive heart failure (R-CHF). In normalcy you do not expect to see hepatic venous branching. This Chou et al. study is available open access and has some interesting, easily readable tables with measurements of the caudal vena cava and presence of gallbladder wall edema.
Watch the “Power of the DH View Webinar” for more information.
Click here for the LINK to the “Power of the DH View” Webinar from March 2022. Please send any comments to Dr. Greg Lisciandro, DVM, DABVP, DACVECC to LearnGlobalFAST@gmail.com
Quiz – Answer is D.
gl/GL 2-27-2023